Submitted by tomrue on
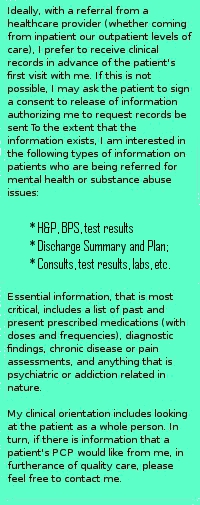
Communication among primary care providers, mental health professionals, and consumers increases patient wellness. When a doctor or other professional refers a patient for psychotherapy or substance abuse counseling, it is important to maintain communication with the mental health counselor. One way to assure this with Choices Mental Health Counseling, PLLC is to fax a simple form or letter to 866-428-0282, rather than just handing the patient a business card or flyer - though also giving the patient a contact number (845-513-5002) may help solidify the referral in his or her mind.
By faxing a referral, an attempt can also be made to reach out to the patient, in addition to leaving the option with the patient to initiate contact.
 Wellness centers on all aspects of health. Eight dimensions of wellness described by the Substance Abuse and Mental Health Administration's "10x10 Wellness Campaign" (www.10x10.samhsa.gov) include physical, emotional, social, intellectual, spiritual, occupational, environmental, and financial.
Wellness centers on all aspects of health. Eight dimensions of wellness described by the Substance Abuse and Mental Health Administration's "10x10 Wellness Campaign" (www.10x10.samhsa.gov) include physical, emotional, social, intellectual, spiritual, occupational, environmental, and financial.
Many times, somatic symptoms closely correlate with mental health issues. For example, in addition to looking for medical causes, physicians should consider possible emotional etiologies for chronic headaches, back pain, muscle aches and joint pain, digestive problems, exhaustion and fatigue, sleeping problems, change in appetite or weight, dizziness or lightheadedness.
Because such symptoms occur with many conditions, many depressed people never get help, because they don't know that their physical symptoms might be caused by depression. A lot of doctors miss the symptoms, too.
By treating the underlying mental health issues, doctors may see less need to medicate physical symptoms and better compliance with medical self-care may result.
Examples include showing up for scheduled healthcare appointments, taking medications as directed, or following up for further return appointments to the doctor.
A recent study found depressed patients with chronic illnesses were less likely to take medications. Noncompliance is a clue that depression could be a cause, the study found.[1]
Evidence shows longer-term effects by cognitive psychotherapy with medication over antidepressants alone.[2]
Other nonpharmacologic interventions often increase the efficacy of antidepressant medications.[3]
A columnist in American Medical News recommends that when treating mental health conditions, primary care providers bill by using the CPT codes measuring the time spent on the visit rather than codes indicating the complexity.
"When [William L.] Bruning's Mid-America Coalition studied reimbursement patterns for depression treatment, it discovered that the evaluation and management codes 99201-99205 for new patients and 99212-99215 for established patients were usually reimbursed when accompanied by the ICD-9 diagnosis codes for the condition. The codes 90801-90899 for psychiatric or psychotherapy services generally were not in the primary care setting," amednews.com advises[4].
The information should be documented in a patient's chart along with the time spent on this subject.
The American College of Preventive Medicine recommends that primary care physicians routinely screen all adults for depression. One in six Americans will experience major depression during their lives. Preventive medicine experts recommend that primary care physicians ask the following two questions. If patients answer "yes" to both, further screening is warranted.[5]
- Over the past month, have you felt down, depressed or hopeless?
- Over the past month, have you felt little interest or pleasure in doing things?
The ripple effects of depressive illness are felt not only by those diagnosed with the disorder; depression has a serious impact on the patient’s family, caregivers, colleagues, and society at large.
A second behavioral health concern for which primary care physicians are well positioned to screen is alcohol and substance abuse. One of the oldest and most popular screening tools for alcohol abuse is the CAGE test, consisting of four questions designed to detect indication of alcohol problems over a lifetime.[6]
- C - Have you ever felt you should cut down on your drinking?
- A - Have people annoyed you by criticizing your drinking?
- G - Have you ever felt bad or guilty about your drinking?
- E - Eye opener: Have you ever had a drink first thing in the AM to steady your nerves or get rid of a hangover?
The same questions can be adapted for other recreational drug use.
At Choices Mental Health Counseling, patients are encouraged to be as truthful and open with their physicians as they are in therapy concerning all the drugs they take, regardless of purpose or source. We want to communicate that we are all on the patient's side.
In the "social history" portion of a doctor's history and physical exam, questions about family should include specific inquiries about history of mental illness or chemical dependence. Another public health epidemic to be addressed at the same time history or ongoing intimate partner violence victimization, which questions such as:
- Have you ever been slapped, kicked, or otherwise physically hurt by your partner?
- Are you currently in a relationship with a person who threatens or physically hurts you?
- Have you ever been forced to have sexual activities?
- Has anyone ever forced you to have sexual activities that made you feel uncomfortable?
In cases where victimization is ongoing, a top priority should be discussing a basic safety plan with the patient, for use when she or he decides that it is time (and that it is safe) to leave the abusive environment. Included in such a plan should be important phone numbers (police, hotlines, friends, domestic violence shelter), knowing how to get out of the residence in a hurry if things get out of hand; having basic necessities, including cash, available; ideas about where to go and how to get there without a car (such as a friend who agrees to help); making an extra set of important papers; and avoiding leaving a trail of clues for the abuser to follow, such as long distance-calls from home; and alerting schools, courts, and agencies not to give out any information on children or the victim.
In some instances, patients may be receptive to the idea of therapy for post-traumatic stress symptoms, or related depression or anxiety. However, it is important not to pathologize the victim, but rather to offer the option of counseling as a potentially useful support.
In relationships where violence is ongoing, marriage or couples counseling is usually contra-indacated, as it may jeapordize the victim's safety even further.
Individual counseling for the victim might be of value, but top priorities are personal safety and respecting the victim's right to choose whether or when it is safe, including for children, to leave. When children are involved, mandatory reporting of suspected child abuse or maltreatment may come into play.
According to Pavan and Drife (2004), "Estimates of the prevalence of childhood sexual abuse among the general population vary from 7% to 38% but among gynaecological patients rates are generally between 15% and 20%. Rates are highest among women with chronic pelvic pain and those who have had gynaecological surgery. Childhood sexual abuse may cause adult depression, somatisation or neurological changes."
More than this, a significant body of research demonstrates high positive correlations between histories of childhood sexual abuse and more than just gynecological complaints[7], but frequent use of the healthcare system as an adult, ranging from emergency room visits, internal medicine, opthamology visits[8], type II diabetes[9], as well as many other "leading causes of death in adults"[10].
[1] Grenard JL, et al. (2011). "Depression and Medication Adherence in the Treatment of Chronic Diseases in the United States: A Meta-Analysis", Journal of General Internal Medicine, published online May 1 (PMID:21533823).
[2] Hensley PLm et al. (2004). "Long-term effectiveness of cognitive therapy in major depressive disorder", Depression and Anxiety, 20(1):1-7 (PMID:15368590).
[3] Harvard Mental Health Letter (2011). "Mindfulness may rival medication at preventing depression relapse," March; 27(9):7 (PMID:21480550).
[4] Victoria Stagg Elliott (2011). "Treating mental illness in primary care -- and still getting paid", American Medical News, March 14 (ama-assn.org/amednews/2011/03/14/bica0314.htm).
[5] Kshamica Nimalasuriya, K (2009). "Screening adults for depression in primary care: A position statement of the American College of Preventive Medicine," Journal of Family Practice, October, 58(10):535-538 (www.jfponline.com/pages.asp?aid=8010)
[6] Mayfield D, et al. (1974). "The CAGE Questionnaire: Validation of a New Alcoholism Screening Instrument", American Journal of Psychiatry, October, (ajp.psychiatryonline.org/cgi/content/abstract/131/10/1121).
[9] Pavan K and Drife J (2004). Childhood sexual abuse and subsequent gynaecological conditions, The Obstetrician & Gynaecologist, 6:209–214. link
[8] Newman MG (2000). The relationship of childhood sexual abuse and depression with somatic symptoms and medical utilization, Cambridge University Press. (PMID: 12027043) link
[9] Rich-Edwards, J (2010). Abuse in Childhood and Adolescence As a Predictor of Type 2 Diabetes in Adult Women, American Journal of Preventive Medicine, 39(6)529–536, published online November 9. link
[10] Felitti VJ (1998). "Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study", American Journal of Preventive Medicine, 14(4), link
